Introduction
Delirium, an acute cognitive disorder characterized by fluctuating mental status and inattention, is a prevalent condition among older adults admitted to hospital settings. Its manifestation is associated with detrimental outcomes, including prolonged length of stays, increased mortality rates, and a significantly elevated risk of developing incident dementia in the long term.1,2 Despite its clinical significance, previous research has highlighted the concerning issue of poor recognition and documentation of delirium at the time of admission when proactive screening measures are lacking.3–6
Recognizing this challenge, Waikato Hospital in New Zealand, a tertiary, teaching hospital with 600 inpatient beds, took proactive steps to update its Delirium Guidelines in 2023. The revised guidelines suggested the implementation of the 4AT (Rapid Assessment Test for Delirium) as an initial screening tool for all patients aged 65 years and above upon hospital admission, as suggested by the NICE Guidelines.7,8 This initiative aimed to enhance the early identification of delirium and cognitive impairment, facilitating timely interventions and appropriate care planning.
Method
To evaluate the effectiveness of this quality improvement measure, an internal audit (CASU 4488P) was conducted across two inpatient wards over four weeks during March 2024. Admission notes and 4AT assessments were reviewed retrospectively. During the implementation phase, a dedicated Consultation-Liaison Psychiatry nurse provided support and guidance to ward nurses, assisting them in conducting daily assessments of newly admitted patients aged 65 years and older to two Older Persons and Rehabilitation wards using the validated 4AT according to the https://www.the4at.com user guide. Clinical delirium suspicion without a formal assessment was assessed by reviewing CHART-DEL (chart-based delirium instrument) trigger words and phrases for delirium identification in the admission records.9
A Microsoft® Excel® for Microsoft 365 MSO (Version 2408 Build 16.0.17928.20114) 64-bit spreadsheet was used for data collation and analysis. Based on the HDEC screening form, the audit was out of scope and did not require HDEC approval.
Results
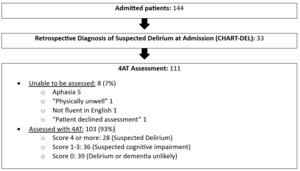
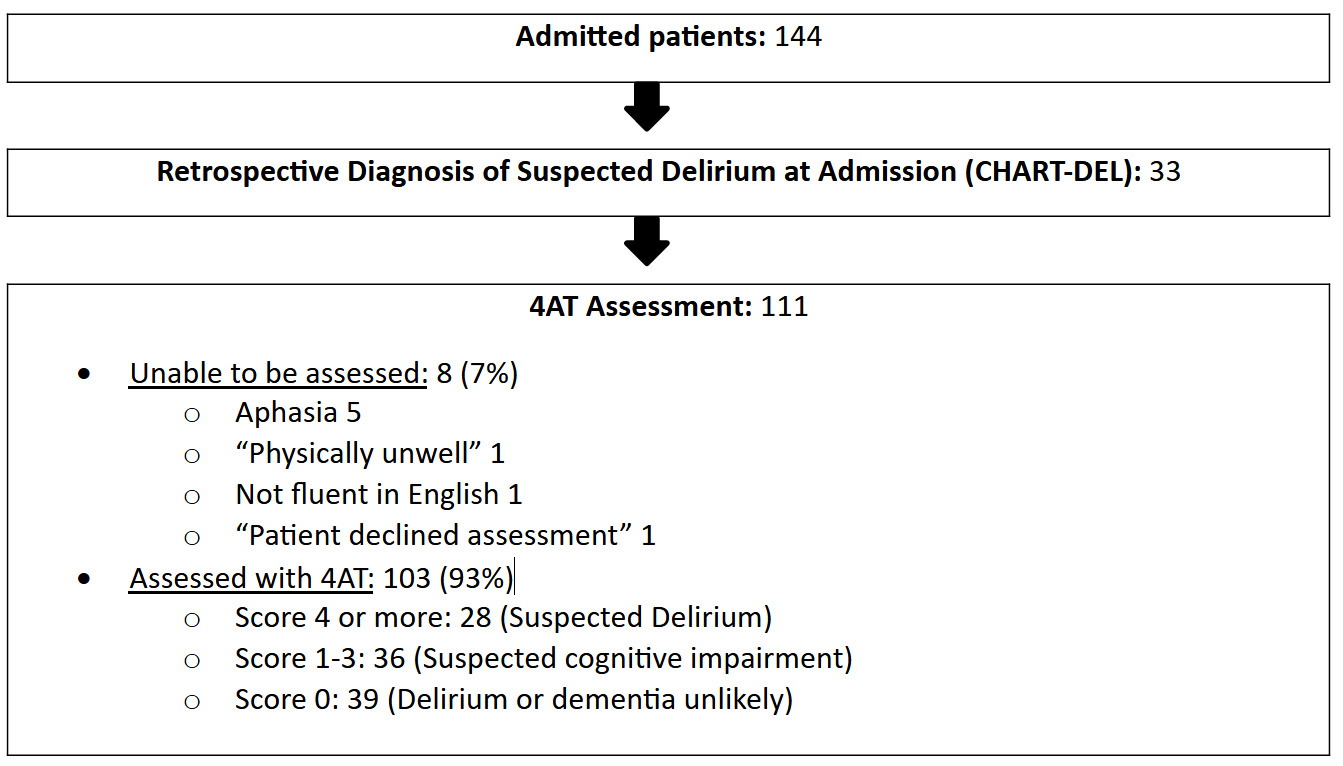
The audit encompassed a total of 144 patients consecutively admitted during the evaluation period (Figure 1). Upon reviewing the admission notes, it was determined that 23% (33/144) of patients already met the criteria for delirium based on the CHART-DEL. This initial finding highlighted the presence of delirium cases among the admitted patient population.
Of the remaining 111 eligible patients who did not meet delirium criteria at admission, 7% could not be assessed using the 4AT due to various factors, such as language impairment. The remaining 103 patients underwent the 4AT assessment by ward nursing staff within 72 hs from admission, with 27% (28/103) meeting the criteria for suspected delirium and 35% (36/103) exhibiting signs of suspected cognitive impairment.
The audit revealed a significant increase in the detection rate of suspected delirium at admission, rising from the initial 23% (33/144) before the formal assessment (based on CHART-DEL) to 42% (61/144) after the implementation of the 4AT screening tool. Moreover, the audit identified a substantial number of patients who did not meet the criteria for delirium but were at an increased risk due to underlying cognitive impairment. Remarkably, only 1.4% (2/144) of patients had a documented history of cognitive impairment at admission, and both individuals met the criteria for delirium based on their 4AT scores.
Previous research has shown that patients who cannot be assessed for delirium have poorer outcomes (e.g., length of stay and mortality) compared to patients with a negative delirium screening.10 If these 8 patients are added to the 36 patients identified with suspected cognitive impairment, a total of ~30.5% (44/144) of the patients in this study can be classified as high risk for developing delirium.
Discussion
Our audit provides compelling evidence that implementing formal delirium assessment tools, particularly the 4AT, during the admission process for older adults significantly improves detection of this critical clinical presentation. This structured approach not only enhances the identification of existing delirium cases but also enables the recognition of patients at increased risk of developing delirium during hospitalization. This early recognition facilitates timely intervention and implementation of preventive measures, potentially reducing delirium-associated complications and mortality. Additionally, the data confirmed poor documentation of premorbid cognitive function across the assessed cases, aligning with findings previously noted in local research by Rodwell and colleagues.3
The clinical significance of these findings cannot be overstated, considering delirium affects up to 50% of hospitalized older adults and is associated with increased mortality, extended hospital stays, and higher rates of institutional care placement. Despite its prevalence and serious consequences, delirium remains frequently undetected in routine clinical practice without systematic screening protocols, with an estimated 50-75% of cases going undiagnosed. Our audit demonstrates how structured assessment tools can bridge this critical gap in clinical care.
Previous studies have demonstrated that adherence to the 4AT is high and sustainable in hospital settings, with Alhaidari and Matsis11 finding consistent implementation rates of 76-89% over extended periods. Their research also revealed that most barriers to completing the assessment were potentially avoidable with proper training, clear institutional protocols, and targeted staff support. Common barriers included time constraints, uncertainty about tool interpretation, and lack of standardized documentation procedures—all addressable through comprehensive implementation strategies.
The practicality of the 4AT merits particular attention. Considering that it takes, on average, less than 2 minutes to administer and can be completed by both nursing staff and house officers without specialized training, its implementation represents a feasible and cost-effective addition to standard admission protocols. The tool’s simplicity and brevity make it particularly suitable for busy clinical environments where efficiency is paramount.
Our findings align with emerging evidence regarding the effectiveness of delirium screening tools in various clinical settings. Vonnes and Tofthagen12 demonstrated in their quality improvement project that routine delirium screening in hospitalized oncology patients resulted in a 28% reduction in delirium-associated complications and a 15% decrease in length of stay. Similarly, Bauernfreund and colleagues13 reported that implementing systematic delirium screening in acute medical units led to earlier detection and intervention, with subsequent improvements in patient outcomes.
In conclusion, this audit highlights the significant positive impact of implementing systematic delirium screening protocols, such as the 4AT, in enhancing delirium detection and risk stratification among hospitalized older adults. By proactively identifying patients at risk, healthcare professionals can initiate timely interventions, optimize care planning, and potentially mitigate the adverse outcomes associated with delirium. The evidence from previous studies demonstrates that early identification can lead to better care pathways and improved clinical outcomes for patients with delirium.12,13
For sustained improvement, however, organizational considerations must be addressed. It is worth noting that evidence shows that while the implementation of short-term supervised interventions can successfully increase the rate of delirium detection, this rate tends to revert to pre-intervention levels after the supervision phase ends.14 This suggests that maintaining improved practice requires ongoing education, regular audit cycles, and institutional commitment to delirium assessment as a quality standard.
The findings underscore the value of integrating evidence-based screening tools into routine clinical practice, paving the way for improved patient outcomes and quality of care for this vulnerable population. Moving forward, we recommend developing comprehensive implementation strategies that include regular staff education, clear documentation protocols, and periodic quality assessment to ensure sustained adherence to delirium screening practices. Additionally, future research should focus on evaluating the long-term impact of systematic delirium screening on patient outcomes, healthcare utilization, and cost-effectiveness across diverse clinical settings.
Conflict of interest
The authors declare that there is no conflict of interest.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.